Fluid intelligence and crystallized intelligence are two concepts of human intelligence that play distinct roles in mental processing and knowledge application. Fluid intelligence (gf) refers to the capacity to reason quickly and think abstractly, enabling individuals to solve novel problems without relying on prior knowledge. It reflects cognitive abilities essential for logical reasoning, pattern recognition, and…
Toxic RNA Interference May Play Key Role in Alzheimer’s
Significant neuronal degeneration is one consequence of Alzheimer’s disease, which is projected to impact approximately 6.7 million Americans in 2023. However, the mechanisms underlying neuron death remain inadequately comprehended. According to a new Northwestern Medicine study, RNA interference may be a crucial factor in Alzheimer’s disease. Scientists have identified brief strands of toxic RNAs that…
What is the Illusion of Validity?
The illusion of validity is a cognitive bias that occurs when individuals overestimate the predictive accuracy of their judgments when analyzing data, especially in the presence of seemingly strong evidence. It leads them to believe that their ability to predict outcomes is valid when it may not be. Crucially, this phenomenon can persist even in the face…
Does Reading Help Your Brain? Cognitive Benefits of Reading
Reading, one of the most complex cognitive procedures, has a significant impact on the brain, influencing its structure, activity, and connectivity. It engages numerous brain regions and facilitates the enhancement of various brain functions. Research into the neurological benefits of reading has demonstrated increases in brain activity, especially in areas associated with language comprehension and processing. Studies…
Which Parts of CBT for Insomnia are Most Beneficial?
The benefits of cognitive behavioral therapy for insomnia (CBT-I) are maximized, according to new research, through the use of a combination of cognitive and behavioral strategies, optimally administered in person by a therapist. CBT-I, a variant of talk therapy, may be administered via self-help manuals or in-person sessions. Through the examination of 241 studies encompassing…
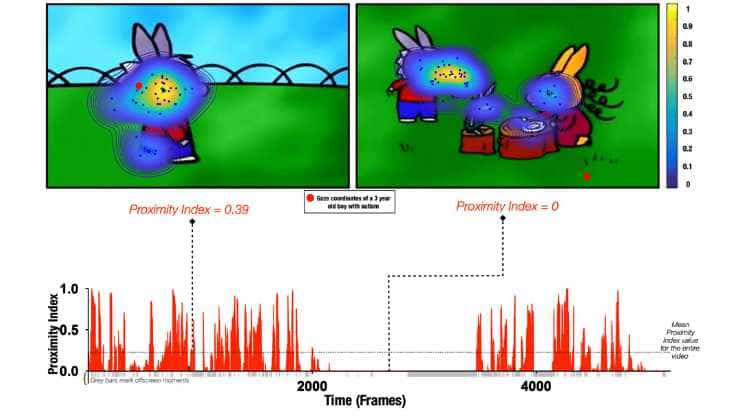
Social Attention Develops Differently in Individual Autistic Children
As they grow, children’s attention shifts to social factors in their surroundings, such as faces or social interactions. However, children with autism are frequently more engaged in non-social stimuli, such as textures or geometric shapes. By tracking where children look while viewing a cartoon, researchers at Université de Genève have revealed that attention in autistic…
Inflammation Links Stress to Metabolic Syndrome
Lifestyle and genetics, as well as a variety of other factors both within and outside of our control, are known to play a role in the development of metabolic syndrome, a group of conditions that increase the risk of serious health problems. A new study has discovered that stress, due to its proclivity to increase…
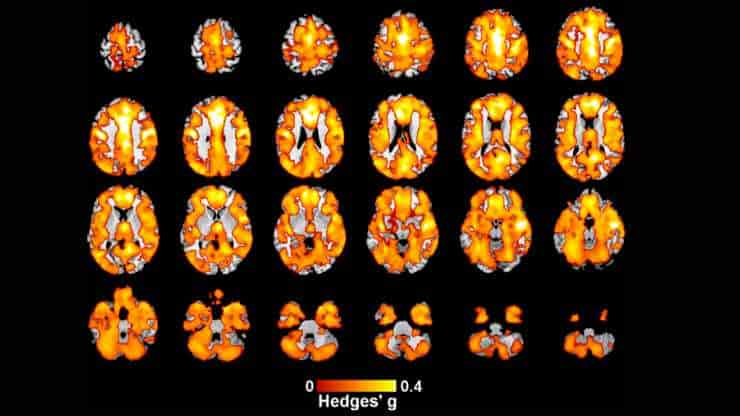
Early Onset Psychosis Linked With Reduced Brain Gray Matter
A new study from the Institute of Psychiatry, Psychology, and Neuroscience has discovered a link between a decrease in gray matter in the brain and early onset psychosis (EOP). The research, the largest brain imaging study ever conducted in EOP, offers unparalleled amounts of data regarding the illness. It demonstrates that, in comparison to other…
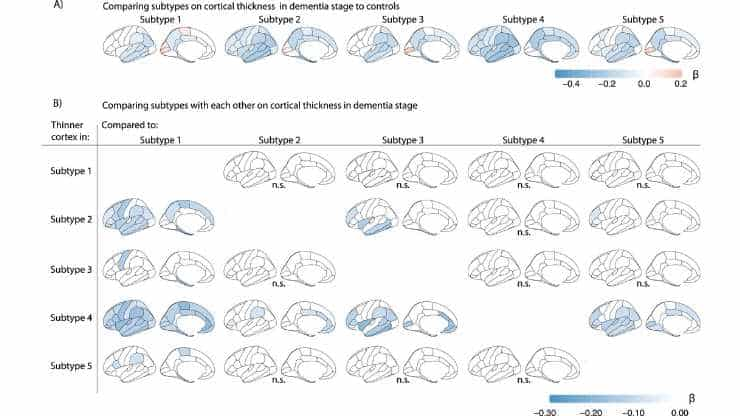
Five Alzheimer’s Disease Biological Variants Identified
Five biochemical varieties of Alzheimer’s disease have been uncovered by Dutch researchers, each of which may require a different treatment. As a result, previously studied medications may look ineffective or only marginally effective. This is the conclusion of Alzheimer Center Amsterdam researcher Betty Tijms and colleagues from Amsterdam UMC and Maastricht University. Amyloid and tau…