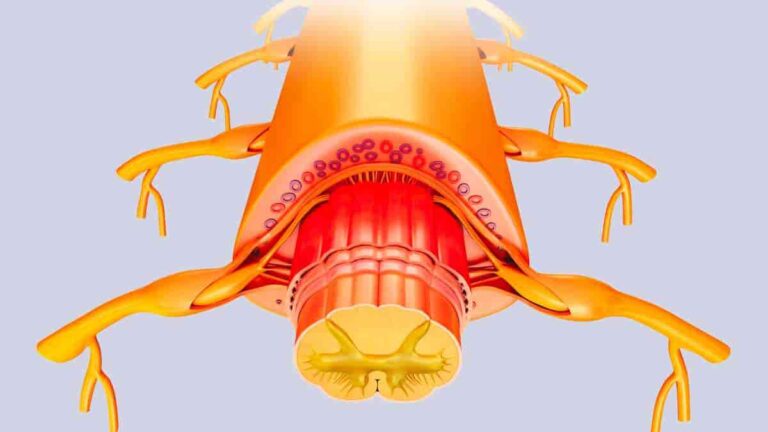
Electrical stimulation of the spinal cord is feasible, well-tolerated, and has therapeutic potential for treating depression, according to a pilot clinical trial led by University of Cincinnati researchers at the Lindner Center of HOPE.The research of principal investigator Francisco Romo-Nava, MD, Ph.D., focuses on how the brain-body connection is involved in psychiatric disorders. “We think…
Evidence Does Not Support Love Languages Role in Relationships
Even if you don’t know what your personal love language is, you’ve probably heard of it. The theory’s popularity in mainstream culture has only grown in the 30 years after Baptist pastor Gary Chapman published “The Five Love Languages: The Secret to Love That Lasts.” However, psychology researchers at the University of Toronto Mississauga recently…
Long Term Potentiation
Long-term potentiation (LTP), in neuroscience, refers to a persistent strengthening of synapses based on recent patterns of activity. These are synaptic activity patterns that result in a long-term increase in signal transmission between two neurons. Long-term depression, the inverse of LTP, results in a long-term decline in synaptic strength. It is one of several mechanisms…
Base Rate Fallacy: Understanding and Overcoming Cognitive Bias
In probability judgments, ignoring the base rates can lead to errors called the base rate fallacy. This occurs when people fail to consider the base rates while assessing the likelihood of an event or attribute happening. Instead, they rely on specific information about a case, causing them to overlook the fundamental probabilities derived from a broader…
Cartesian Mindset an Alternative For Resisting Disinformation
When it comes to dealing with disinformation, relying exclusively on trust or distrust mindsets isn’t the most successful strategy. While trust frequently leads to the acceptance of erroneous information and distrust can serve as a barrier against it, both mindsets have limitations. Professor Ruth Mayo of the Hebrew University of Jerusalem offers a novel take…
Understanding the Representativeness Heuristic
The representativeness heuristic is a mental shortcut that helps individuals make judgments by comparing the similarity of new information to existing mental prototypes. According to prototype theory, we generate these prototypes based on our experiences and use them as a reference point for evaluation and decision-making. When using the representativeness heuristic, individuals often overestimate the probability of occurrence…
Cannabis-related Psychiatric Disorders Are On the Rise
The increased potency and pervasive use of cannabis (marijuana) are associated with an increase in cannabis-related psychiatric disorders, according to a new review article published in the New England Journal of Medicine by the University of Maryland School of Medicine (UMSOM). It emphasizes the critical necessity for physicians to promptly identify and manage patients exhibiting…
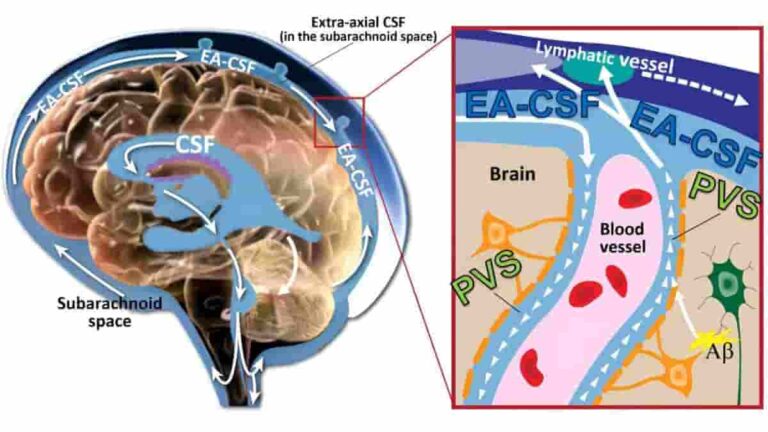
Expanded Perivascular Spaces in Infant Brains Linked to Raised Risk of Autism
Researchers at the University of North Carolina at Chapel Hill have found that infants with abnormally enlarged perivascular spaces have a 2.2 times greater chance of developing autism than infants with the same genetic risk. Their study also found that increased perivascular gaps in infancy are linked to sleep disorders seven to ten years later.…
The Availability Heuristic Cognitive Bias
The availability heuristic is a cognitive bias that influences the way individuals perceive the frequency or likelihood of an event based on the ease with which relevant instances come to mind. A heuristic in psychology is a mental shortcut, allowing people to make quick judgments and decisions without investing significant cognitive resources into evaluating every…