Researchers at the University of North Carolina at Chapel Hill have found that infants with abnormally enlarged perivascular spaces have a 2.2 times greater chance of developing autism than infants with the same genetic risk. Their study also found that increased perivascular gaps in infancy are linked to sleep disorders seven to ten years later.
“These results suggest that perivascular spaces could serve as an early marker for autism,”
said Dea Garic, Ph.D., of the UNC School of Medicine’s Department of Psychiatry. Garic co-led the study with Mark Shen, Ph.D.
The researchers looked at newborns who were at a higher risk for developing autism because they had an older sibling who had autism. They monitored these infants from 6 to 24 months of age, before autism was diagnosed.
Their study found that 30% of infants who later developed autism had enlarged perivascular spaces by 12 months. By 24 months of age, nearly half of the infants diagnosed with autism had enlarged perivascular spaces.
Cerebrospinal Fluid and Sleep
There has been a revival of study on the critical activities of cerebrospinal fluid (CSF) in regulating brain health and development over the last ten years.
Shen’s lab was the first to demonstrate that increased CSF volume was seen in infants with autism at 6 months of age. Excessive CSF volume at 6 months was connected to larger perivascular gaps at 24 months, according to the current study.
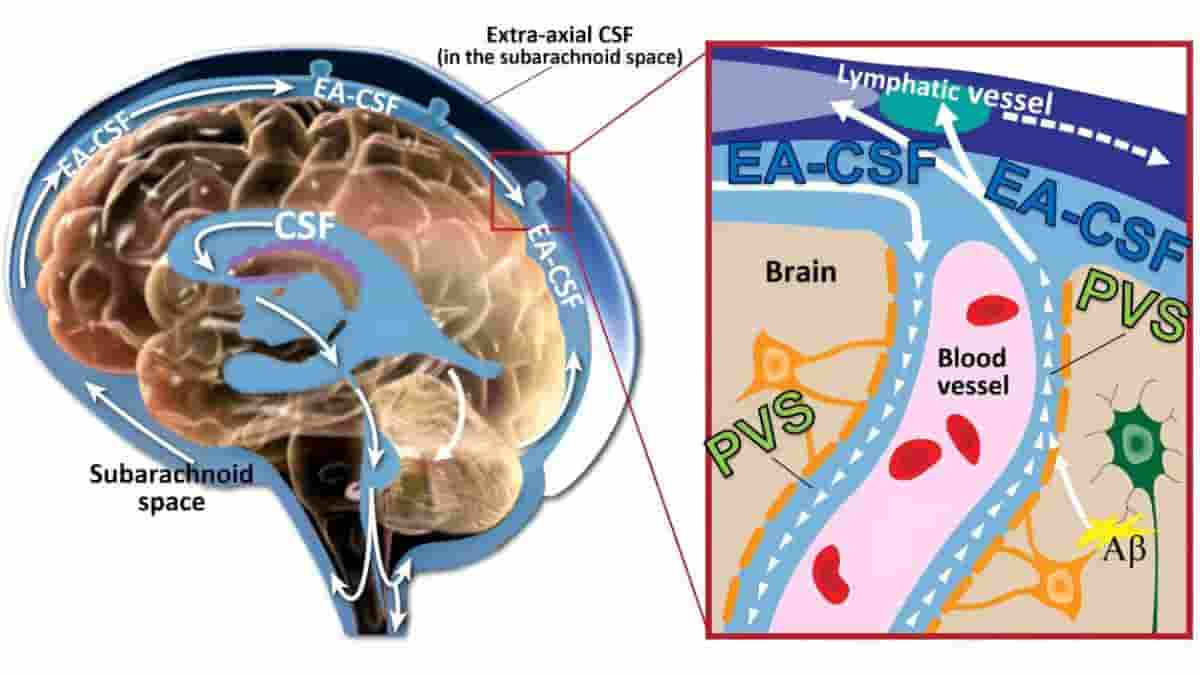
Every six hours, the brain expels a wave of CSF that runs through perivascular gaps, removing potentially damaging neuroinflammatory substances like amyloid beta from the brain. Because the majority of CSF circulation and clearance happens when we sleep, the cerebrospinal fluid cleansing process is highly efficient.
Disrupted sleep, however, can reduce CSF clearance from perivascular spaces, leading to dilation or enlargement, but this has previously only been studied in animal studies or in human studies of adults. This is the first study of its kind in children.
Based on previous research, Shen, the paper’s senior author, and Garic expected that CSF abnormalities in infancy would be linked to later sleep disorders. According to the current sleep study, children with increased perivascular spaces at two years of age had a greater rate of sleep disruptions when they reached school age.
“Since autism is so highly linked with sleep problems, we were in this unique position to examine CSF dynamics and sleep. It was really striking to observe such a strong association separated by such a long period of time over childhood. But it really shows how perivascular spaces not only have an effect early in life, but they can have long-term effects, too.”
said Garic, the first author of the paper.
Enlarged Infant Perivascular Spaces
The research was done in conjunction with the Infant Brain Imaging Study (IBIS), a nationwide network of researchers investigating brain development, autism, and related developmental disabilities. The network consists of five universities, of which the University of North Carolina-Chapel Hill is the lead site.
Garic and Shen examined 870 MRIs from IBIS to determine excessive CSF volume and expanded perivascular gaps for their investigation. MRIs were taken from babies during natural sleep at six, twelve, and twenty-four months of age to track changes over time.
The infant’s brain undergoes rapid development over this period. Previously, measurement of perivascular spaces was only thought to be clinically relevant for disorders of aging in older adults, such as in dementia. These findings suggest that younger populations may need to be considered and monitored for these types of brain abnormalities.
“Our findings were striking, given that neuroradiologists typically view enlarged perivascular spaces as a sign of neurodegeneration in adults, but this study reported it in toddlers. This is an important aspect of brain development in the first years of life that should be monitored,”
said Garic.
Next Steps
Garic and Shen hypothesize that excess cerebrospinal fluid volume is stagnant or clogged and not circulating through the brain as efficiently as it should.
The researchers intend to next use MRIs to measure CSF in a sleeping infant’s brain again, but this time to focus on the physiology and speed of cerebrospinal fluid flow throughout the brain.
The research team is also working with other collaborators to quantify the size of perivascular spaces and the severity of behavioral outcomes. The team also plans to extend their research to neurogenetic syndromes associated with autism, such as Fragile X syndrome and Down syndrome.
“Collectively, our research has shown that CSF abnormalities in the first year of life could have downstream effects on a variety of outcomes, including later autismdiagnosis, sleep problems, neuroinflammation, and possibly other developmental disabilities,”
said Shen.
Abstract
Importance: Perivascular spaces (PVS) and cerebrospinal fluid (CSF) are essential components of the glymphatic system, regulating brain homeostasis and clearing neural waste throughout the lifespan. Enlarged PVS have been implicated in neurological disorders and sleep problems in adults, and excessive CSF volume has been reported in infants who develop autism. Enlarged PVS have not been sufficiently studied longitudinally in infancy or in relation to autism outcomes or CSF volume.
Objective: To examine whether enlarged PVS are more prevalent in infants who develop autism compared with controls and whether they are associated with trajectories of extra-axial CSF volume (EA-CSF) and sleep problems in later childhood.
Design, Setting, and Participants: This prospective, longitudinal cohort study used data from the Infant Brain Imaging Study. Magnetic resonance images were acquired at ages 6, 12, and 24 months (2007-2017), with sleep questionnaires performed between ages 7 and 12 years (starting in 2018). Data were collected at 4 sites in North Carolina, Missouri, Pennsylvania, and Washington. Data were analyzed from March 2021 through August 2022.
Exposure: PVS (ie, fluid-filled channels that surround blood vessels in the brain) that are enlarged (ie, visible on magnetic resonance imaging).
Main Outcomes and Measures: Outcomes of interest were enlarged PVS and EA-CSF volume from 6 to 24 months, autism diagnosis at 24 months, sleep problems between ages 7 and 12 years.
Results: A total of 311 infants (197 [63.3%] male) were included: 47 infants at high familial likelihood for autism (ie, having an older sibling with autism) who were diagnosed with autism at age 24 months, 180 high likelihood infants not diagnosed with autism, and 84 low likelihood control infants not diagnosed with autism. Sleep measures at school-age were available for 109 participants. Of infants who developed autism, 21 (44.7%) had enlarged PVS at 24 months compared with 48 infants (26.7%) in the high likelihood but no autism diagnosis group (P = .02) and 22 infants in the control group (26.2%) (P = .03). Across all groups, enlarged PVS at 24 months was associated with greater EA-CSF volume from ages 6 to 24 months (β = 4.64; 95% CI, 0.58-8.72; P = .002) and more frequent night wakings at school-age (F = 7.76; η2 = 0.08; P = .006).
Conclusions and Relevance: These findings suggest that enlarged PVS emerged between ages 12 and 24 months in infants who developed autism. These results add to a growing body of evidence that, along with excessive CSF volume and sleep dysfunction, the glymphatic system could be dysregulated in infants who develop autism.
Reference:
- Garic D, McKinstry RC, Rutsohn J, et al. Enlarged Perivascular Spaces in Infancy and Autism Diagnosis, Cerebrospinal Fluid Volume, and Later Sleep Problems. JAMA Netw Open. 2023; 6(12):e2348341. doi:10.1001/jamanetworkopen.2023.48341
Image credit: JAMA Network Open (2023). DOI: 10.1001/jamanetworkopen.2023.48341