Changes in brain patterns that shape trust behaviour can detect depression even when symptoms are still hidden, according to a Hiroshima University study. Brain scans revealed that reduced gray matter volumes in brain regions involved in social cognition linked to a compromised trusting ability shared a link with depression vulnerability that could aid in its early detection.
“Our question was: Can we use social personality information to predict the development of mental disorders, such as depression? Having tools that help identify early signs of mental disorders could accelerate medical or other therapeutical interventions,”
said the study’s corresponding author, Alan S. R. Fermin.
Delayed Depression Treatment
Major depressive disorder (MDD), also known as clinical depression, is a widespread mental health condition affecting millions worldwide. Despite serious symptoms that interfere with daily life, many people delay seeking medical help for various reasons, leading to worsened conditions.
When severe symptoms of MDD are present, doctors can easily make a diagnosis. However, treatment can become more difficult at that point as medication response decreases, necessitating more aggressive interventions.
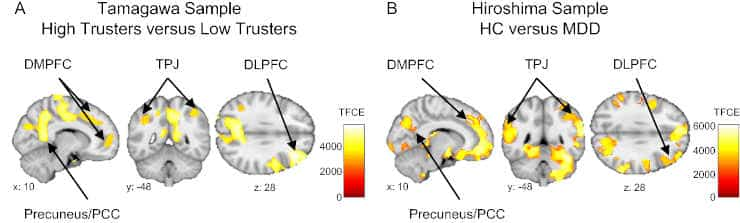
While their findings support previous research that found a link between trust and depression, the researchers in this study were the first to identify the neuroanatomical basis of this relationship.
Low Trust and Depression
Trust is associated with the expectation of kindness, reciprocation of cooperation from others, and compliance with social norms. However, trusting others is difficult because unexpected aversive social interactions, such as gossip or bullying at school, harassment at work, or even physical violence at home, are frequently observed.
Breach of trust and individual differences in trusting others have been shown to harm mental health, with low trusters isolating themselves from social interactions and developing depression as a result.
“In our study, we not only replicated the association between low trust and depression but also demonstrated that brain regions associated with trust were also associated with the degree of depressive symptoms one year in advance,”
Fermin said.
Gray Matter Reduction
Credit: Sci Rep 12, 16724 (2022) CC-BY
Overall, the team observed that the gray matter volume in social cognition-related brain regions was reduced in the brains of individuals with lower levels of trust.
“Also, we found that this gray matter volume reduction among low trusters was similar to the brain of actual depressive patients. Thus, even though our participants hadn’t received any diagnosis of depression, their brains were already showing signs of depression,”
said Fermin.
Low trust and high depressive symptoms are both associated with decreased gray matter volumes in the bilateral precuneus, bilateral angular gyrus, ventromedial prefrontal cortex (right frontal pole and right rectus gyrus), bilateral dorsolateral prefrontal cortex, bilateral dorsomedial prefrontal cortex, and left posterior cingulate cortex. In addition, whole-brain voxel-based morphometry analysis of their study sample revealed that when levels of trust decrease, gray matter volume in the parahippocampus-amygdala region also decreases.
These regions help humans regulate their emotions, think, and predict the mental states and behaviours of others.
Consequently, the decreased volume of these brain regions in individuals with low trust suggests possible disturbances in emotion regulation and the estimation of the trustworthiness of others, which may contribute to the development of depression.
However, what causes these brain regions to shrink remains unknown.
Major Depressive Disorder Vulnerability
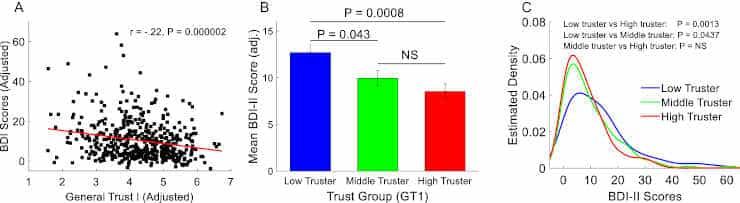
(A) Significant negative correlation between trust (TA1) and depressive symptoms measured up to 17 months apart. (B) Significant higher depressive symptoms in low trusters relative to middle and high trusters. The three groups were created based on their trust scores (TA1). (C) The distribution of depressive symptoms among low trusters was significantly skewed toward higher values relative to middle and high trusters.
Credit: Sci Rep 12, 16724 (2022) CC-BY
To better comprehend the neuroanatomical relationship between trust and depression susceptibility, the researchers examined the gray matter volume of 470 healthy participants from Machida, a Tokyo suburb, using magnetic resonance imaging. The researchers then utilized psychological questionnaires to assess trust, social anxiety, and the size of social networks.
As an indicator of major depressive disorder susceptibility, participants were also asked to self-report any depressive symptoms they might be experiencing using a psychiatric questionnaire.
The researchers recruited 185 outpatients from Hiroshima University Hospital and other Hiroshima Prefecture medical institutions to validate their findings. They examined gray matter volume abnormalities in 81 participants diagnosed with clinical depression to determine whether brain regions associated with trust and depressive symptoms are associated with neuroanatomical abnormalities commonly observed in MDD patients.
“We hope that our findings could support the development of institutional and social policies to increase social trust. For example, at work, school, or public space and prevent the development of mental disorders,”
Fermin said.
The researchers intend to determine which additional personality types could serve as biosocial markers for predicting the onset of mental disorders.
Reference:
- Fermin, A.S.R., Kiyonari, T., Matsumoto, Y. et al. The neuroanatomy of social trust predicts depression vulnerability. Sci Rep 12, 16724 (2022)
Last Updated on November 11, 2023
