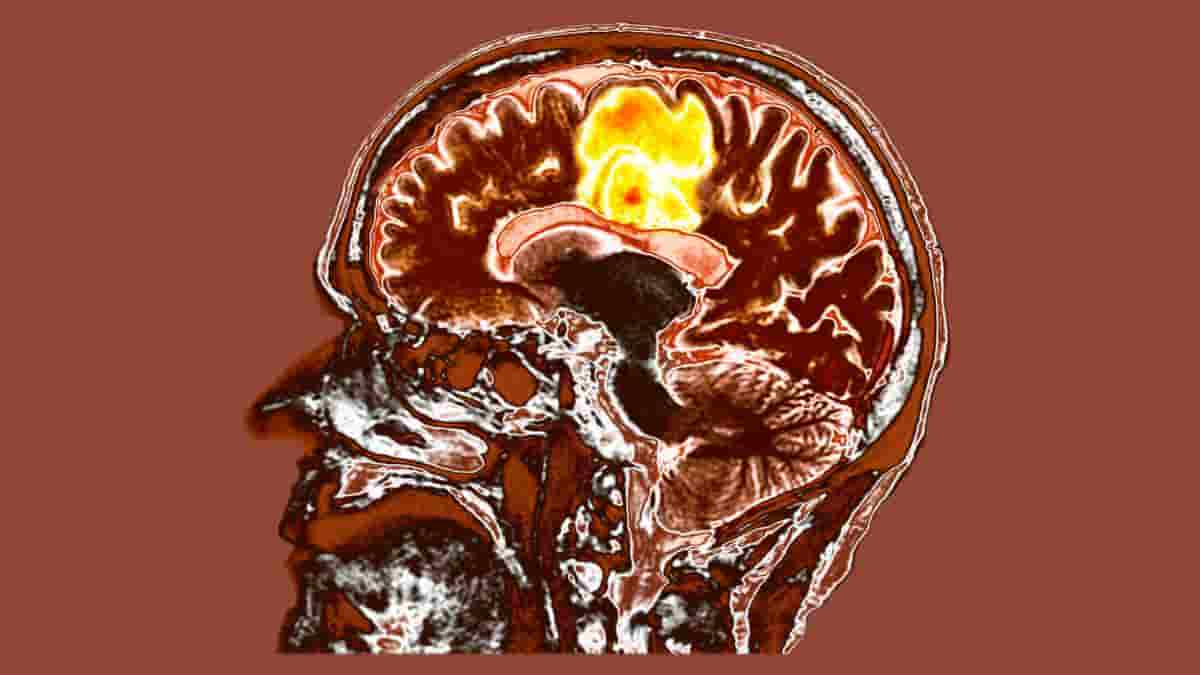
Glioblastoma is one of the most resistant malignancies to therapy, with those diagnosed living for fewer than two years. In a new study, researchers at the University of Notre Dame discovered that an understudied cell could provide fresh insight into how aggressive primary brain cancer resists immunotherapy.
“A decade ago, we didn’t even know perivascular fibroblasts existed within the brain, and not just in the lining of the skull. My lab’s expertise is examining tumors from an engineering and systems-based approach and looking at the novel mechanical features in rare cancers that may have been understudied or overlooked,”
said senior author Meenal Datta, assistant professor of aerospace and mechanical engineering at Notre Dame.
Datta’s lab began analyzing different genes expressed in the tumor microenvironment related to the extracellular matrix — the scaffolding cells create to support future cell adhesion, migration, proliferation, and differentiation — and other cell types using standard bioinformatics and newer AI-based approaches.
Perivascular Fibroblasts
They found an unexpected and relatively new cell type: perivascular fibroblasts. These fibroblasts are normally located in a healthy brain’s blood vessels and deposit collagen to maintain the structural integrity and functionality of brain vessels.
“It was a serendipitous discovery. We started in a completely different direction and stumbled upon this population of cells by using a combination of both bulk and single-cell RNA sequencing analyses of patient tumors.”
said first author Maksym Zarodniuk, graduate student in the TIME (Tumor Immune Microenvironment & Mechanics) Lab and the bioengineering doctorate program.
Researchers were able to identify two groups of patients based on their data: those with a larger proportion of perivascular fibroblasts and those with much less. They discovered that patients with brain cancer who had more perivascular fibroblasts in their tumors were more likely to respond poorly to immunotherapies and have a poor survival outcome.
Immunosuppressive Microenvironment
The researchers determined that perivascular fibroblasts help to create an immunosuppressive tumor microenvironment, helping the cancer to better escape the immune system. By fostering stem-like cancer cells that seldom divide, which are thought to be a key source of tumor relapse and metastasis, the fibroblasts may also help the disease withstand therapies such as chemotherapy that targets dividing cells.
“Moving forward, we want to do new experiments to confirm what we found in this paper and provide some good ground to start thinking about how to improve response to immunotherapy,”
Zarodniuk said.
Because perivascular fibroblasts are part of the vasculature of a healthy brain, Datta believes these cells are breaking off and invading the glioblastoma tumor. Instead of supporting healthy brain function, these fibroblasts are being altered to aid the tumor.
“Most people think about the brain as being very soft, with soft cells and a soft matrix. But by putting down these fibroblasts and making these very fibrous proteins, it gives us an entirely different perspective on the structure of the brain and how it can be taken advantage of by cancer cells originating in the same organ,”
Datta said.
Abstract
Excessive deposition of extracellular matrix (ECM) is a hallmark of solid tumors; however, it remains poorly understood which cellular and molecular components contribute to the formation of ECM stroma in central nervous system (CNS) tumors. Here, we undertake a pan-CNS analysis of retrospective gene expression datasets to characterize inter- and intra-tumoral heterogeneity of ECM remodeling signatures in both adult and pediatric CNS disease. We find that CNS lesions – glioblastoma in particular – can be divided into two ECM-based subtypes (ECMhi and ECMlo) that are influenced by the presence of perivascular stromal cells resembling cancer-associated fibroblasts (CAFs). Ligand-receptor network analysis predicts that perivascular fibroblasts activate signaling pathways responsible for recruitment of tumor-associated macrophages and promotion of cancer stemness. Our analysis reveals that perivascular fibroblasts are correlated with unfavorable response to immune checkpoint blockade in glioblastoma and poor patient survival across a subset of CNS tumors. We provide insights into new stroma-driven mechanisms underlying immune evasion and immunotherapy resistance in CNS tumors like glioblastoma, and discuss how targeting these perivascular fibroblasts may prove an effective approach to improving treatment response and patient survival in a variety of CNS tumors.
Reference:
- Zarodniuk, M., Steele, A., Lu, X. et al. CNS tumor stroma transcriptomics identify perivascular fibroblasts as predictors of immunotherapy resistance in glioblastoma patients. npj Genom. Med. 8, 35 (2023). Doi: 10.1038/s41525-023-00381-w