Proteins involved in the innate immune system may be at the root of amyotrophic lateral sclerosis (ALS), a fatal motor neuron disease, new research from Boston Children’s Hospital and Harvard Medical School suggests.
“The unmet need for therapies for neurodegenerative diseases is huge, and our work opens up a whole new pathology that we could address,”
said co-principal investigator Judy Lieberman, MD, Ph.D., a researcher at Boston Children’s. Despite the availability of medications to slow the progression of neurodegenerative diseases, there are currently no cures.
The discovery of an innate immune molecule that plays a role in neurodegeneration paves the way for new ways of thinking about neuronal health.
Gasdermin E and Pyroptosis
Scientists found that inhibiting a molecule in the brain associated with inflammation prevents cellular damage in human neurons and slows the progression of amyotrophic lateral sclerosis in mice.
When cells detect danger, such as an infection, immune molecules are activated to sound an alarm that recruits and activates immune cells to the site of damage in an attempt to eliminate the threat and coordinate tissue repair. Occasionally, the immune response involves a family of proteins known as gasdermins, which induce cell death through a highly inflammatory process known as pyroptosis.
One type of gasdermin, gasdermin E, is highly expressed in nerve cells in the brain. However, nobody knew what it was doing.
Axon Degeneration
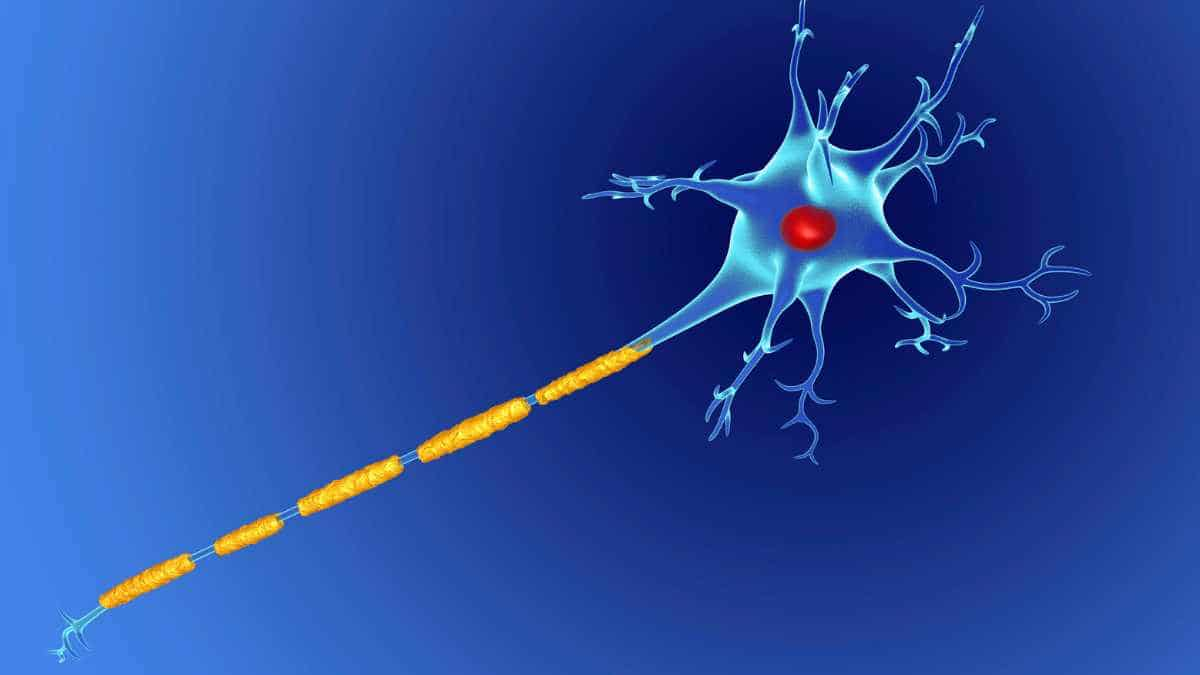
First, the research team, led by Drs. Lieberman and Chiu, investigated the effect of gasdermin E on neurons. The group examined the effects of gasdermin E on axons, or the parts of neurons that transmit electrical signals, using models of neurons derived from mice and human tissue.
The researchers discovered that when neurons detect a threat, the protein gasdermin E causes damage to the mitochondria and axons. Axons degenerate, but cells do not perish.
“If you look at a plate of neurons, you see a jungle of axons. But if you look at a plate where gasdermin E is activated, you see retractions of these cellular processes,”
explained Himanish Basu, a postdoctoral researcher in Chiu’s lab at Harvard University who led this study. This retraction occurs in the nerves of ALS patients’ muscles. ALS is a progressive disease characterized by muscle twitching and weakness, eventually leading to muscle atrophy and paralysis.
Double-edged Sword
To better comprehend the relationship between gasdermin E and neurodegeneration, the team transformed stem cell samples from ALS patients into neurons, creating models of ALS motor neurons.
The researchers discovered that gasdermin E is abundant in these neurons. And by silencing gasdermin E, they could protect axons and mitochondria from damage.
The team wished to determine whether the effects observed in cells could translate to improvements in neurodegeneration-related symptoms. The researchers silenced gasdermin E in a mouse model of amyotrophic lateral sclerosis.
They discovered that it slowed the progression of symptoms and resulted in motor neuron protection, longer axons, and less inflammation overall. These findings suggest that gasdermin E induces neuronal changes that may contribute to the progression of disease.
“Inflammation is a double-edged sword, and could be very destructive based on context,”
said Chiu.
Although some drugs can inhibit the effects of other gasdermins, it is unknown whether gasdermin E can be targeted with drugs. However, this is an essential first step in the development of new ALS treatment methods.
Reference:
- Dylan V Neel, Himanish Basu, Georgia Gunner, Matthew D Bergstresser, Richard M.Giadone, Haeji Chung, Rui Miao, Vicky Chou, Eliza M. Brody, Xin Jiang, Edward B. Lee, Christine Marques, Aaron Held, Brian Wainger, Clotilde Lagier-Tourenne, Yong-JieZhang, Leonard Petrucelli, Tracy L. Young-Pearse, Alice S Chen-Plotkin, Lee L. Rubin, Judy Lieberman, Isaac M Chiu. Gasdermin-E mediates mitochondrial damage in axons and neurodegeneration. Neuron (2023). DOI: 10.1016/j.neuron.2023.02.019