A novel strategy to target autoimmunity in the brain makes treatment safer and more effective by utilizing designer bacteria. Autoimmunity in the brain is central to several diseases, including multiple sclerosis.
In a new study, researchers from Brigham and Women’s Hospital demonstrated the treatment’s potential using preclinical models of these diseases, discovering that the technique offered a more precise way to target brain inflammation with fewer negative side effects than standard therapies.
“Engineered probiotics could revolutionize the way we treat chronic diseases. When a drug is taken, its concentration in the bloodstream peaks after the initial dose, but then its levels go down. However, if we can use living microbes to produce medicine from within the body, they can keep producing the active compound as its needed, which is essential when we consider lifelong diseases that require constant treatment,”
said lead author Francisco Quintana, PhD.
Dendritic Cells
About 5–8% of the population in the U.S. have an autoimmune disease. Even though most of these diseases are common, there aren’t many ways to treat them.
Because of the blood-brain barrier, which separates the brain from the circulatory system, autoimmune diseases that affect the brain, such as MS, are especially difficult to treat. The researchers studied dendritic cells, a type of immune cell abundant in the gastrointestinal tract and the spaces around the brain, to look for new ways to treat autoimmune diseases.
Although these cells assist in immune system regulation, researchers are still unsure of how they relate to autoimmune diseases. The team discovered a biochemical pathway that dendritic cells use to prevent other immune cells from attacking the body by examining dendritic cells in the central nervous system of mice.
Immune System Brakes
The mechanism discovered by the researchers acts like a brake on the immune system.
“In most of us, it’s activated, but in people with autoimmune diseases, there are problems with this brake system, which means the body has no way to protect itself from its own immune system,”
said Quintana.
The scientists discovered that lactate, a molecule involved in numerous metabolic processes, can activate this biochemical brake. The scientists could then genetically modify probiotic bacteria to make lactate.
“Probiotics are nothing new — we’ve all seen them sold as supplements and marketed as a way to promote health. By using synthetic biology to get probiotic bacteria to produce specific compounds relevant to diseases, we can take the benefits of probiotics and amp them up to the max,”
said Quintana.
Leveraging Probiotics
They tested their probiotic in mice with a disease similar to Multiple Sclerosis. They discovered that, despite living in the gut, the bacteria could reduce the effects of the disease in the brain. They found no bacteria in the mice’s bloodstream, implying that the effect they observed was due to biochemical signalling between cells in the gut and the brain.
“We’ve learned in recent decades that the microbes of the gut have a significant impact on the central nervous system. One of the reasons we focused on multiple sclerosis in this study was to determine whether we can leverage this effect in treating autoimmune diseases of the brain. The results suggest we can,”
said Quintana.
Although the current study only looked at the effect of the probiotic on mice, the researchers are optimistic that the approach could be easily translated into the clinic because the strain of bacteria used to create the probiotic has already been tested in humans.
The researchers are also working to improve their method for treating autoimmune diseases that affect other parts of the body, particularly gut diseases like inflammatory bowel syndrome.
“The ability to use living cells as a source of medicine in the body has tremendous potential to make more personalized and precise therapies. If these microbes living in the gut are powerful enough to influence inflammation in the brain, we’re confident we’ll be able to harness their power elsewhere as well,”
said Quintana.
Reference:
- Sanmarco, L.M., Rone, J.M., Polonio, C.M. et al. Lactate limits CNS autoimmunity by stabilizing HIF-1α in dendritic cells. Nature (2023)
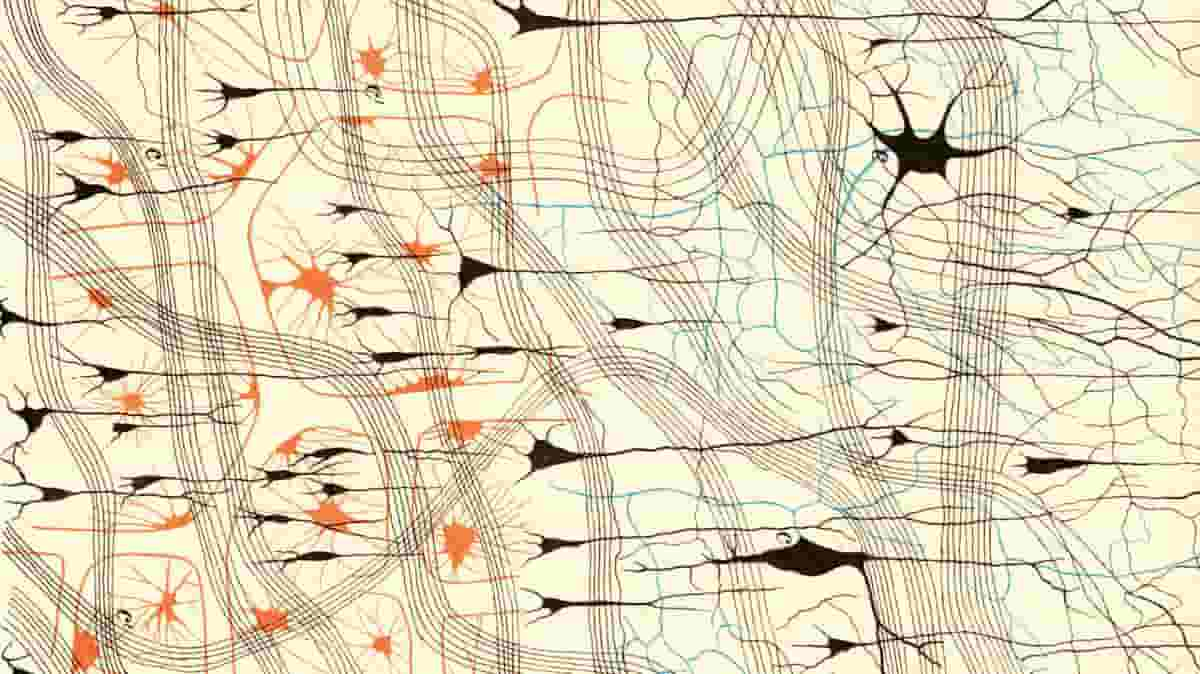
Top Image: Nerve cells in a dog’s olfactory bulb (detail), from Camillo Golgi’s Sulla fina anatomia degli organi centrali del sistema nervoso (1885)