Postoperative delirium, a syndrome of confusion that often appears in the first few days following surgery, affects up to 40% of elder surgery patients. Postoperative delirium has been linked to extended hospital stays, severe distress, and major postoperative consequences, although the underlying causes remain unknown.
Previous research in mice suggested that postoperative delirium could be caused by changes in the blood-brain barrier, a layer of cells in the blood arteries of the brain that prevents drugs from entering the brain. Large-scale human investigations in this region were not possible due to technological difficulties in measuring the barrier.
This new study overcomes those limitations. It also shows that patients who had lower performance on cognitive tests prior to surgery were more likely to experience postoperative delirium.
“These findings are significant because we now have a roadmap to tackle a problem that impacts millions of older adults in the US every year. If we can find a way to prevent the blood-brain barrier from opening after surgery or figure out what is passing through this barrier and getting to the brain, we can work to develop a therapy that may prevent postoperative delirium,”
said corresponding author Michael Devinney, assistant professor in the department of anesthesiology at Duke University School of Medicine.
CSF to Plasma Albumin Ratio
To arrive at these findings, scientists examined more than 200 patients, ages 60 or older, before and after non-cardiac and non-neurological surgeries. To understand changes in the blood-brain barrier’s permeability, they collected spinal fluid and blood samples before surgery and 24 hours after, measuring the ratio of a protein called albumin to cerebrospinal fluid as an indicator of the barrier’s fluidity.
Credit: Ann Neurol. doi: 10.1002/ana.26771 CC-BY
The research team also wanted to control for cognitive ability as a risk factor for delirium. To do so, they administered extensive cognitive evaluations before and after surgery.
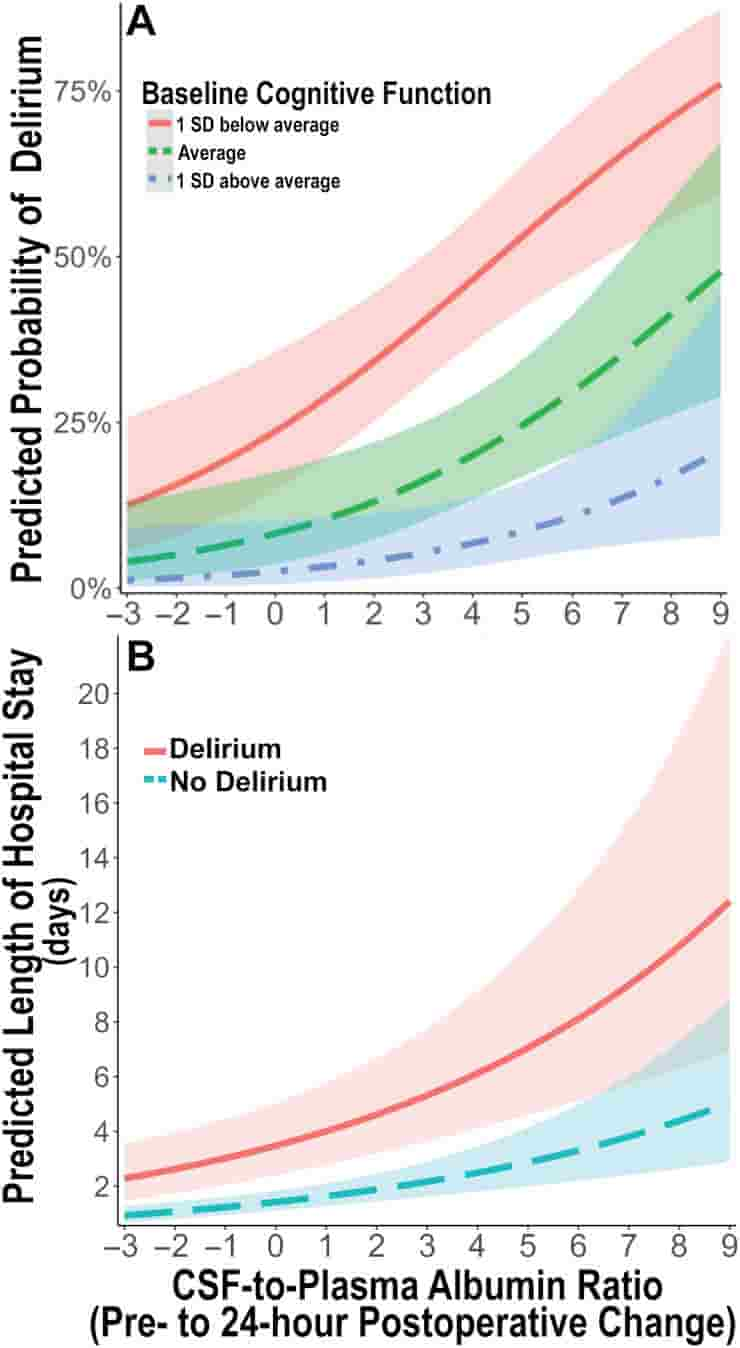
They found that increased blood-brain barrier permeability is associated with greater delirium rates and longer hospital stays amongst all patients, suggesting that the permeability increase is a response to surgery.
They also found that those with lower cognitive abilities experienced increased delirium rates. However, the lower performance on cognitive testing affected delirium risk separate from postoperative blood-brain barrier opening.
Two-hit Model
The work suggests that there may be a two-hit model for postoperative delirium.
“It appears to involve both a predisposing factor such as impaired preoperative cognition, and a precipitating factor involving postoperative blood-brain barrier dysfunction,”
Devinney said.
It is known that inflammatory molecules can pass through a leaky blood-brain barrier and cause cognitive impairments. Devinney says researchers are already planning a follow-up study to take a closer look at the collected spinal fluid samples to see if particular inflammatory factors are present in higher concentrations amongst patients who experienced delirium.
The study received funding from the National Institutes of Health, the Duke Department of Anesthesiology, the Foundation for Anesthesia Education and Research, the Society of Neuroscience in Anesthesiology and Critical Care, and the International Anesthesia Research Society.
Abstract
Objective
Although animal models suggest a role for blood–brain barrier dysfunction in postoperative delirium-like behavior, its role in postoperative delirium and postoperative recovery in humans is unclear. Thus, we evaluated the role of blood–brain barrier dysfunction in postoperative delirium and hospital length of stay among older surgery patients.
Methods
Cognitive testing, delirium assessment, and cerebrospinal fluid and blood sampling were prospectively performed before and after non-cardiac, non-neurologic surgery. Blood–brain barrier dysfunction was assessed using the cerebrospinal fluid-to-plasma albumin ratio (CPAR).
Results
Of 207 patients (median age = 68 years, 45% female) with complete CPAR and delirium data, 26 (12.6%) developed postoperative delirium. Overall, CPAR increased from before to 24 hours after surgery (median change = 0.28, interquartile range [IQR] = −0.48 to 1.24, Wilcoxon p = 0.001). Preoperative to 24 hours postoperative change in CPAR was greater among patients who developed delirium versus those who did not (median [IQR] = 1.31 [0.004 to 2.34] vs 0.19 [−0.55 to 1.08], p = 0.003). In a multivariable model adjusting for age, baseline cognition, and surgery type, preoperative to 24 hours postoperative change in CPAR was independently associated with delirium occurrence (per CPAR increase of 1, odds ratio = 1.30, 95% confidence interval [CI] = 1.03–1.63, p = 0.026) and increased hospital length of stay (incidence rate ratio = 1.15, 95% CI = 1.09–1.22, p < 0.001).
Interpretation
Postoperative increases in blood–brain barrier permeability are independently associated with increased delirium rates and postoperative hospital length of stay. Although these findings do not establish causality, studies are warranted to determine whether interventions to reduce postoperative blood–brain barrier dysfunction would reduce postoperative delirium rates and hospital length of stay.
Reference:
- Devinney, M.J., Wong, M.K., Wright, M.C., Marcantonio, E.R., Terrando, N., Browndyke, J.N., Whitson, H.E., Cohen, H.J., Nackley, A.G., Klein, M.E., Ely, E.W., Mathew, J.P., Berger, M. and (2023). Role of Blood–Brain Barrier Dysfunction in Delirium following Non-cardiac Surgery in Older Adults. Ann Neurol. doi: 10.1002/ana.26771
