Deep brain stimulation in a relatively novel target area has been demonstrated to alleviate involuntary tremors in Parkinson’s disease and Essential Tremor for at least five and ten years respectively, following therapy beginning. Furthermore, by using this target area, the operation might be performed under general anesthesia. This is demonstrated in Rasmus Stenmark Persson’s thesis at Ume University.
Deep Brain Stimulation (DBS) entails permanently implanting one or two electrodes in distinct target areas of the brain as well as a neuropacemaker beneath the skin on the chest. Continuous electrical stimulation can be used to correct abnormal signal patterns in the brain and relieve symptoms such as tremors.
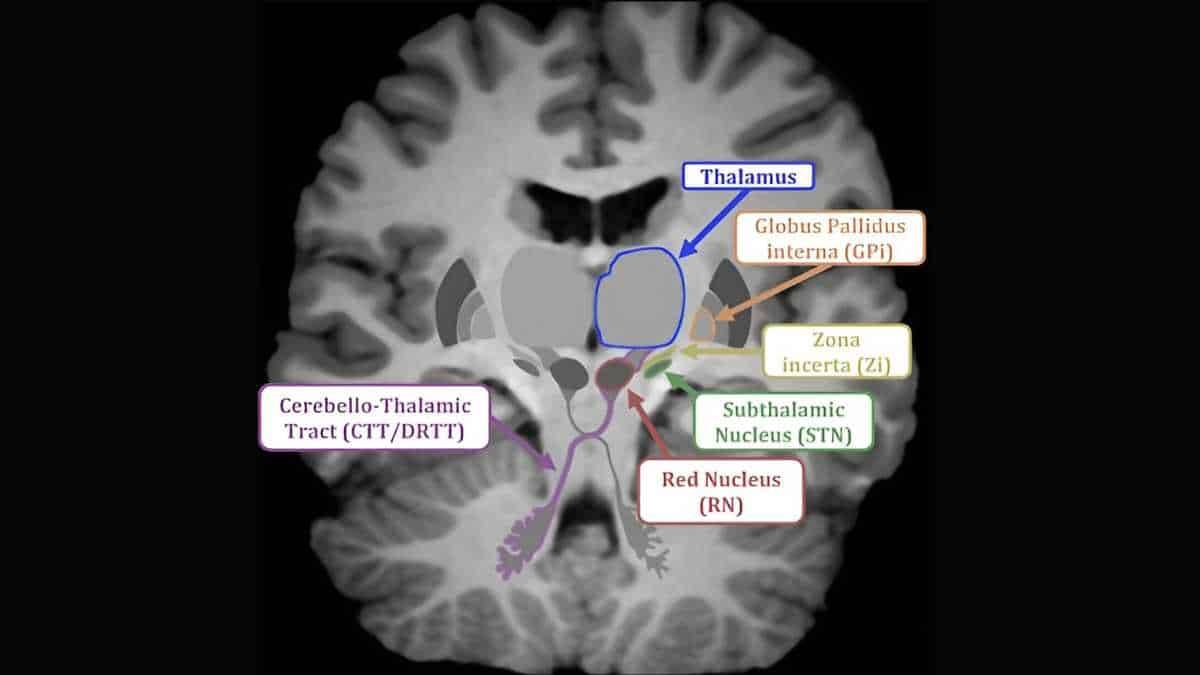
The thalamus, the typical target of tremors, is not detectable on magnetic resonance imaging (MRI). DBS surgery for tremors is typically performed while the patient is awake in order to check proper electrode placement using, among other things, test stimulation.
Caudal Zona Incerta Stimulation
In patients with Parkinson’s disease and essential tremor, DBS that targets a novel structure known as the caudal zona incerta (cZi) alleviates tremors and improves fine motor skills, according to a number of smaller studies.
Since the cZi is located in close proximity to structures visible on MRI, it is possible to confirm a good electrode position with the help of X-rays, which enables surgery under general anesthesia. However, these studies have been conducted with non-blinded evaluations, without a control group and with relatively short follow-up, which limited the scientific strength of the results of these studies.
Now, in a randomized, blinded therapy research, the favorable effect of cZi-DBS on motor symptoms and quality of life in Parkinson’s disease patients was proven for the first time. cZi-DBS had a very positive effect on tremors, a modest influence on fine motor abilities, and an overall positive effect on quality of life.
“In two long-term studies, we saw that the tremors were significantly alleviated for at least five years after surgery for patients with Parkinson’s disease and 10 years for Essential Tremor. We also analyzed the one-year result of cZi-DBS for essential tremor and compared patients who underwent awake surgery with those who underwent surgery under general anesthesia and saw similar effects and complications between the different surgical methods,”
said Persson, set to defends his thesis at Umeå University on Friday, 8 December.
More Accurate Targeting
The stimulation was focused in a region that includes both the zona incerta and neighboring neuronal pathways from the cerebellum to the thalamus, according to a survey. These brain circuits have previously been implicated in the disease process behind tremors in both Parkinson’s disease and essential tremor.
“By analyzing the position of the electrode in the brain and creating simulations of the electric field around the electrodes, we were able to map which structures were affected by the stimulation,”
Persson said.
A more objectively confirmed efficacy of cZi-DBS in Parkinson’s disease means that there is now an additional target area to use for DBS in this disease. For the first time, it has been shown that the effect on the tremors lasts for several years after surgery, even for essential tremor.
Using cZi as a target for DBS rather than the conventional target in the thalamus offers a number of benefits, in addition to comparable efficacy between awake and anesthetized surgery.
“We believe that the fact that the surgery is performed under general anesthesia can increase the accuracy of the operation, potentially reduce complications and improve the experience of the surgery for the patients,”
explained Persson.
Image: Coronal view of the brain with key anatomical structures involved in DBS for PD and ET. For clarity the structures have been placed in the same plane, but it should be noted that some are in different locations in the anteroposterior direction than shown here. Credit: Rasmus Stenmark Persson, Umeå University