Long-term exposure to periodontal disease bacteria causes inflammation and degeneration of neurons in mice that is similar to the effects of Alzheimer’s disease in humans, according to a new study from researchers at the University of Illinois at Chicago.
The findings suggest that periodontal disease, a common but preventable gum infection, may kick start Alzheimer’s, which currently has no treatment or cure.
“Other studies have demonstrated a close association between periodontitis and cognitive impairment, but this is the first study to show that exposure to the periodontal bacteria results in the formation of senile plaques that accelerate the development of neuropathology found in Alzheimer’s patients. This was a big surprise. We did not expect that the periodontal pathogen would have this much influence on the brain, or that the effects would so thoroughly resemble Alzheimer’s disease,”
said Dr. Keiko Watanabe, professor of periodontics at the UIC College of Dentistry and corresponding author on the study.
Amyloid Beta Accumulation
To study the impact of the bacteria on brain health, the Watanabe and her colleagues — including Dr. Vladimir Ilievski, UIC research assistant professor and co-author on the paper — established chronic periodontitis, which is characterized by soft tissue damage and bone loss in the oral cavity, in 10 male wild-type mice.
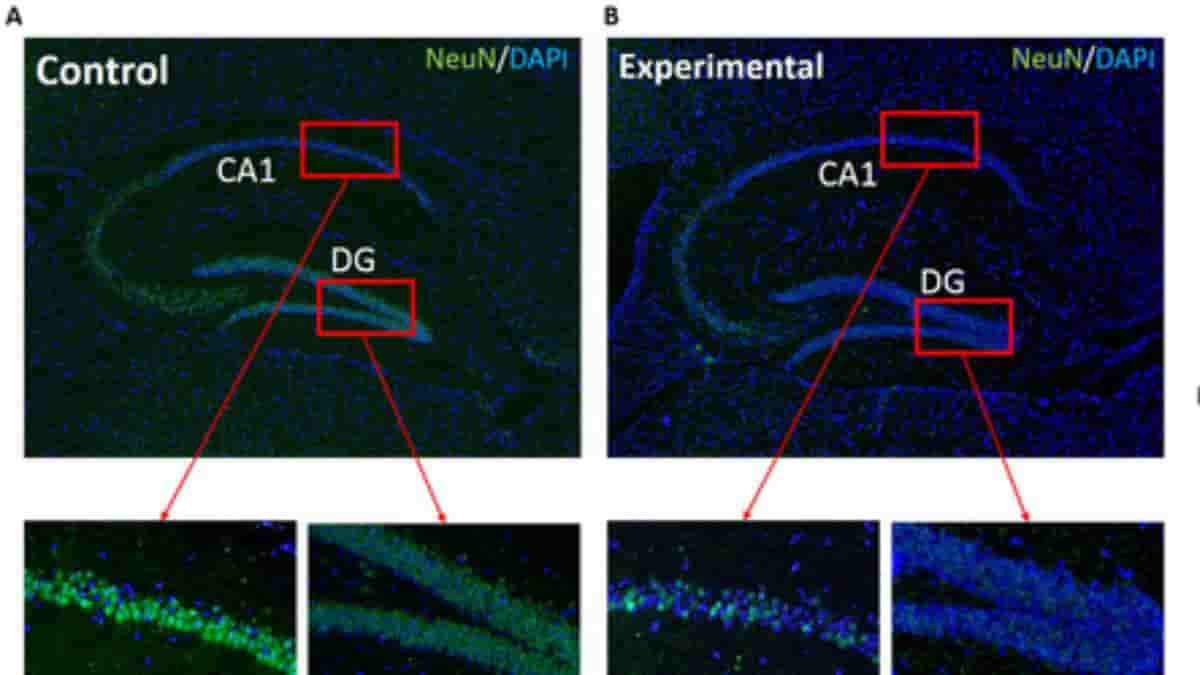
Another ten mice served as the control group. After 22 weeks of repeated oral application of the bacteria to the study group, the researchers studied the brain tissue of the mice and compared brain health.
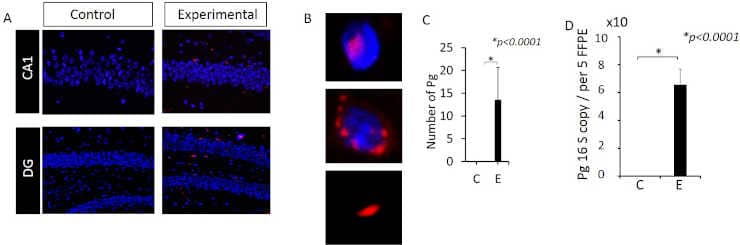
(A) Immunofluorescence microscopy. Red: Pg, Blue: DAPI.
(B) Images showing intra-, peri- and extra-cellularly localized Pg.
(C) Number of Pg/gingipain detected per field (220μm X 160μm). N = 9 mice for experimental and N = 10 mice for control group.
(D) Copy number of Pg 16S RNA genes detected in genomic DNA isolated from 5FFPE samples/mouse, N = 5 mice/group. Y- axis: number of Pg/gingipain per field for (C) and copy number of 16S rRNA genes from genomic DNA for (D). X-axis: C (control), E (experimental) group.
Credit: Vladimir Ilievski et al. CC-BY.
The researchers found that the mice chronically exposed to the gram-negative periodontal pathogen, Porphyromonas gingivalis (Pg) had significantly higher amounts of accumulated amyloid beta — a plaque found in the brain tissue of Alzheimer’s patients. The study group also had more brain inflammation and fewer intact neurons due to degeneration.
Periodontitis is considered a risk factor for dementia and Alzheimer’s Disease (AD), based on a close association between the presence of periodontitis and cognitive impairment/dementia in humans.
Movement Of Periodontal Bacteria
These findings were further supported by amyloid beta protein analysis, and RNA analysis that showed greater expression of genes associated with inflammation and degeneration in the study group. DNA from the periodontal bacteria was also found in the brain tissue of mice in the study group, and a bacterial protein was observed inside their neurons.
“Our data not only demonstrate the movement of bacteria from the mouth to the brain, but also that chronic infection leads to neural effects similar to Alzheimer’s,”
Watanabe said.
The researchers say these findings are powerful in part because they used a wild-type mouse model; most model systems used to study Alzheimer’s rely on transgenic mice, which have been genetically altered to more strongly express genes associated with the senile plaque and enable Alzheimer’s development.
“Using a wild-type mouse model added strength to our study because these mice were not primed to develop the disease, and use of this model gives additional weight to our findings that periodontal bacteria may kick-start the development of the Alzheimer’s,”
Watanabe said.
The researchers say that understanding causality and risk factors for the development of Alzheimer’s is critical to the development of treatments, particularly when it comes to sporadic, or late-onset disease, which constitutes more than 95 percent of cases and has largely unknown causes and mechanisms.
Because females appear to be more vulnerable to Alzheimer’s than males future studies should be conducted to examine the effect of the Pg/gingipain bacteria in female mice also.
Reference:
- Ilievski V, Zuchowska PK, Green SJ, Toth PT, Ragozzino ME, Le K, et al. Chronic oral application of a periodontal pathogen results in brain inflammation, neurodegeneration and amyloid beta production in wild type mice. PLoS ONE 13(10): e0204941. doi: 10.1371/journal.pone.0204941
Top Image: The level of NeuN expression is lower in experimental mice compared with control mice. Images (A &B) are representative of NeuN detected by immunofluorescence microscopy. Credit: PLoS ONE 13(10): e0204941
Last Updated on November 11, 2023