Normative social influence is a basic concept in social psychology that describes how individuals conform to the expectations of others to be accepted or liked. It is a type of social influence leading to conformity and adherence to social norms – the implicit or explicit rules a group has for the acceptable behaviors, values, and…
Social Contagion of Memory: Memory Conformity
Social contagion of memory, also known as memory conformity, refers to the process by which an individual’s memory becomes aligned with the memories or suggestions of others. This alignment may occur consciously or unconsciously and can lead to shared but potentially inaccurate memories across a group. The work on this topic suggest that through social influence, false or…
What is Behavioral Confirmation – Social Perception and Social Reality
Behavioral confirmation is a social psychological term that describes how people’s expectations about others can lead to the confirmation of those expectations through social interaction. This process implicates both the perceiver, who holds certain expectations, and the target, whose behavior may be influenced as a result. In the literature, the phenomenon of belief creating social reality is known…
Imagination Inflation: Memory’s Creative Expansion
Imagination inflation occurs when individuals develop greater confidence in the truth of an event after imagining it, potentially leading to the formation of false memories. The term often relates to childhood memories, as these are typically more malleable and susceptible to misconceptions. Several factors have been linked to an increase in the imagination inflation effect. Imagining a fictitious…
What is State-Dependent Memory: Context in Recall
State-dependent memory refers to when a person’s ability to recall information is influenced by their particular mental or physical state state at the time of encoding the memory. If the internal state during recall matches the state during encoding, retrieval of the memory is typically more successful. This cognitive psychology concept highlights the tight interplay…
Social Exchange Theory: Relationship Reciprocity and Costs
Social exchange theory is a conceptual framework that has its roots in various disciplines, including social psychology, sociology, and economics. It posits that social behavior is a consequence of an exchange process. The goal of these exchanges is to maximize benefits and minimize costs. Psychologist George Homans is a key figure in the development of this theory, laying…
Batson’s Empathy-altruism Hypothesis and Prosocial Behavior
The empathy-altruism hypothesis posits a direct relationship between empathy and altruistic behavior. Originating from the work of social psychologist C. Daniel Batson, this concept suggests that feeling empathy for others can lead to genuine selfless helping actions. Batson has published experimental research to support the empathy-altruism hypothesis ruling out various other egoistic explanations. The hypothesis…
The Atkinson-Shiffrin Model of Memory: Multi-store Memory
The Atkinson-Shiffrin model of memory, formulated by psychologists Richard Atkinson and Richard Shiffrin, offers a structured illustration of the human information processing system. First proposed in 1968, the model includes three main components: Sensory memory: A temporary repository that captures all sensory information, where most of it is lost unless attention is directed to it. Short-term store:…
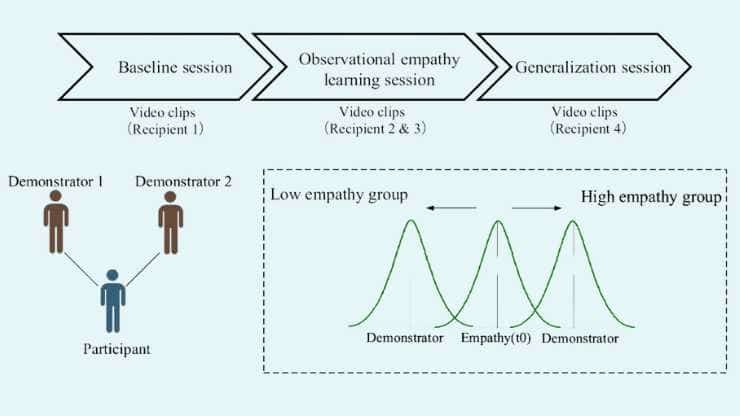
Empathy Transmission Via Observational Reinforcement Learning
In addition to their genetic predispositions, it appears that adults, like children, are able to acquire empathetic reactions from close caregivers. A new study has found that adults can learn to be more or less empathetic by watching others. Prof. Dr. Grit Hein, professor of Translational Social Neuroscience at the Center of Mental Health of…