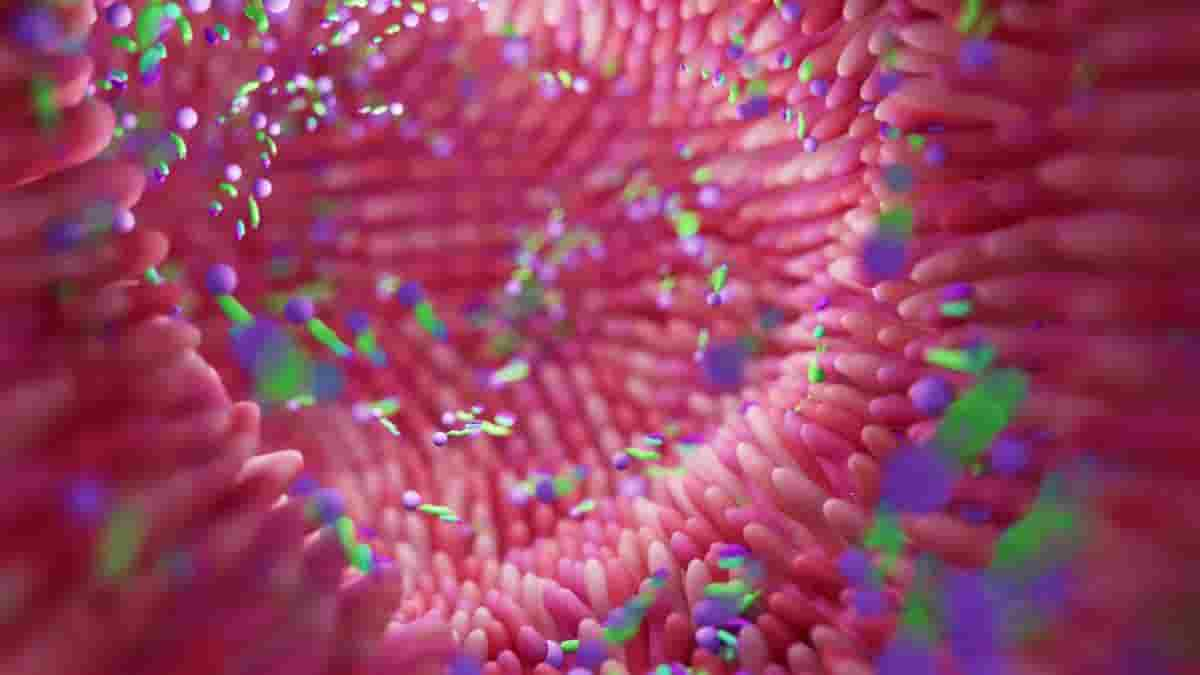
A team led by Johns Hopkins Medicine researchers has identified a specific intestinal immune cell that influences the gut microbiome, which in turn may affect brain functions linked to stress-induced disorders such as depression in mice and humans. Targeting changes mediated by these immune cells in the gut with drugs or other therapies could lead to new treatments for depression.
“The results of our study highlight the previously unrecognized role of intestinal gamma delta T cells in modifying psychological stress responses, and the importance of a protein receptor known as dectin-1, found on the surface of immune cells, as a potential therapeutic target for the treatment of stress-induced behaviors,”
said senior author Atsushi Kamiya, M.D., Ph.D., professor of psychiatry and behavioural sciences at the Johns Hopkins University School of Medicine.
Dectin-1 and Gamma Delta T-cells
Dectin-1 binds to specific antigens or proteins to activate immune cells in specific ways. According to the researchers, this receptor may be involved in altering the microbiome and immune-inflammatory responses in the colon of mice, implying that it may be involved in stress responses via gamma delta T-cells in the intestinal immune system.
Based on previous research linking immune inflammatory responses in the gut to depression, Kamiya and his colleagues devised experiments to investigate stress-induced behaviours caused by an imbalance in the gut microbiota — types of microorganisms found in a specific environment, such as bacteria, fungi, and viruses.
The researchers investigated the effects of chronic social defeat stress (CSDS) on the gut microbiota in mice. CSDS is a common rodent test used to study stress-related disorders such as depression.
Gut Microbiota Diversity
The researchers conducted a series of experiments that simulated potential stress-inducing environments that could mimic similar responses in human environments. Following each exposure, the mice were evaluated and classified as stress-resilient (stress had no negative impact on social interactions) or stress-susceptible (stress increased social avoidance).
Fecal samples were then collected and genetically analyzed to determine the diversity of bacteria in the mice’s gut microbiota.
The analysis revealed that the intestinal organisms in stress-susceptible mice were less diverse than those in stress-resilient mice. It was discovered that stress-susceptible mice had lower levels of Lactobacillus johnsonii (L. johnsonii), a type of probiotic, or “good” bacteria, than stress-resilient mice.
“We found that stress increased the gamma delta T cells, which in turn increased social avoidance However, when the stressed mice were given L. johnsonii, social avoidance decreased and the gamma delta T cells went to normal levels, suggesting that CSDS-induced social avoidance behavior may be the result of lower levels of the bacteria and gamma delta T cell changes,”
said lead author Xiaolei Zhu, M.D., Ph.D., assistant professor of psychiatry and behavioral sciences.
Pachyman Eases Social Avoidance
The researchers investigated how changes in dectin-1 on CSDS-induced elevation of gamma delta T cells responded to pachyman in search of potential natural approaches for depression prevention that are rooted in the gut. Pachyman, a compound extracted from wild mushrooms, is used in Eastern medicine as a natural anti-inflammatory agent and to treat depression.
Mice were given a dose of pachyman, which has been shown in previous research to affect immune function. Flow cytometry data showed that dectin-1 binds to pachyman, inhibiting CSDS-induced gamma delta 17 T cell activity and alleviating social avoidance behavior.
The researchers investigated the makeup of gut organisms in people with major depressive disorder (MDD) compared to people without MDD to gain insight into how changes in the gut microbiota could impact the human brain.
Lactobacillus Relative Abundance
From June 2017 to September 2020, 66 people aged 20 and up were recruited at Tokyo’s Showa University Karasuyama Hospital, Keio University Hospital, and Komagino Hospital.
32 of the study participants had MDD (17 women and 15 men). The control group consisted of the remaining 34 participants (18 women and 16 men) who did not have major depressive disorder.
All study participants had comprehensive evaluations, including a psychiatric history and standard screening assessments for depression and anxiety. Higher scores in these assessments indicate more depressive symptoms.
The diversity of intestinal bacteria was not different between the subjects with MDD and the control group, according to genetic analysis of stool samples.
However, the researchers found that the relative abundance of Lactobacillus was inversely related to higher depression and anxiety scores in the MDD group, implying that the more Lactobacillus found in the gut, the lower the risk of depression and anxiety.
“Despite the differences of intestinal microbiota between mice and humans, the results of our study indicate that the amount of Lactobacillus in the gut may potentially influence stress responses and the onset of depression and anxiety,”
said Kamiya.
More research is needed, the researchers say, to better understand how gamma delta T cells in the intestinal immune system affect neurological functions in the brain, as well as the role of dectin-1 in other cell types along the gut-brain connection under stress conditions.
Reference:
- Zhu, X., Sakamoto, S., Ishii, C. et al. Dectin-1 signaling on colonic γδ T cells promotes psychosocial stress responses. Nat Immunol (2023) DOI: 10.1038/s41590-023-01447-8
Last Updated on August 14, 2023