Combining new brain scan techniques with patient information about any early life trauma can predict with unprecedentedly high (80%) accuracy whether a depressed patient is likely to recover with anti-depressant medications (ADM), or not, a team of Australian and United States mental health researchers has found.
The ability to predict ADM response is important because, up until now, the prescription by doctors of one kind of anti-depressant medication over another has been largely guesswork and finding the right drug treatment can take years. The research, was led by a team at Stanford University, headed by Professor Leanne Williams.
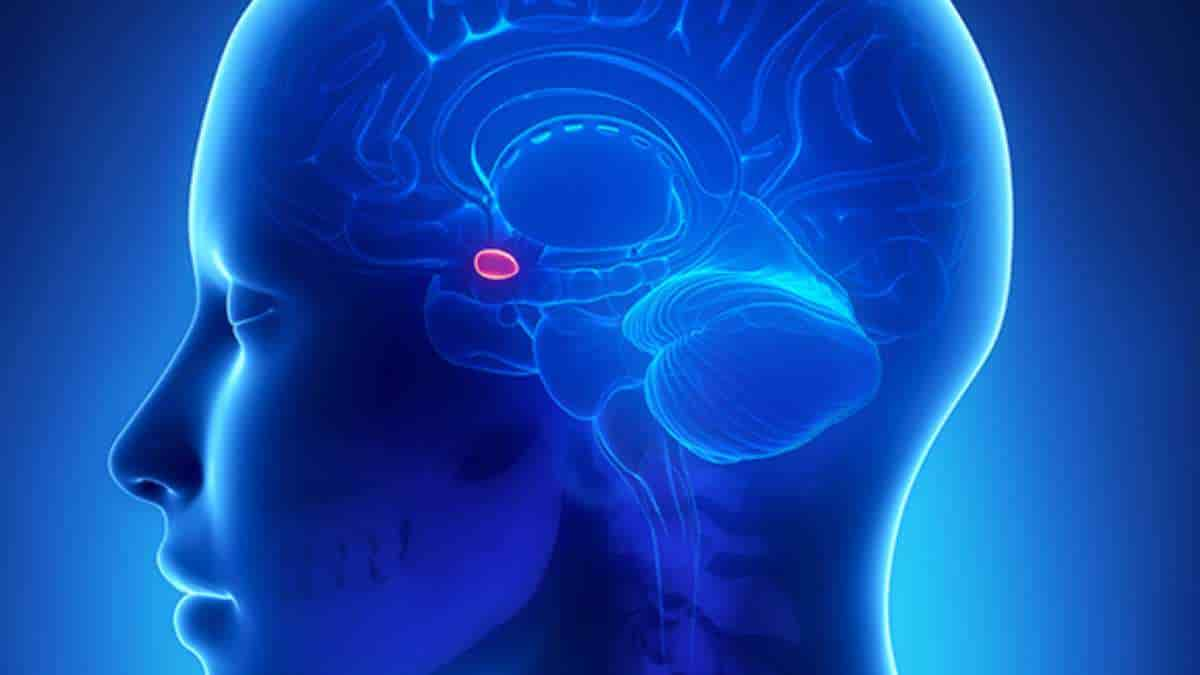
Study participants lay in a functional MRI machine while viewing images of happy faces and fearful faces on a screen in front of them. Each face triggered brain circuits involving the amygdala, the main area of the brain responsible for evaluating and generating emotions.
The findings were based on data from 80 patients collected by The Westmead Institute for Medical Research in Sydney as part of the International Study to Predict Optimized Treatment in Depression (iSPOT-D).
Impaired Amygdala
Co-author Dr Mayuresh Korgaonkar said:
“We know from previous research that the relative reactivity of the amygdala is strongly associated with depression. In simple terms, if your amygdala is impaired you are more vulnerable to suffer from depression. We also know that high levels of exposure to early life stress (ELS) can impact on the amygdala, physically damaging the area – and its ability to moderate emotional response.”
Director of The Westmead Institute’s Brain Dynamics Centre, Dr Korgaonkar, worked with Professor Williams on the MRI data collection for iSPOT-D.
The MRI scans were conducted both before and after an eight-week treatment period with three commonly used antidepressants: sertraline (Zoloft), escitalopram (Lexapro) and venlafaxine (Effexor).
Participants also completed a 19-item questionnaire on ELS, which assessed exposure to abuse, neglect, family conflict, illness or death (or both), and natural disasters prior to the age of 18.
The researchers analyzed the pre-treatment imaging and the questionnaire to predict how the individual patients would respond immediately after the eighth week.
Using a statistical analysis called predictive modelling, study results showed that participants exposed to a high level of ELS were most likely to recover with antidepressants if the amygdala was reactive to the happy faces.
Early Life Stress
Those with a high level of early life stress whose amygdala showed low reactivity to the happy faces were less likely to recover with antidepressants. This research finding is an important step towards giving clinicians the first objective diagnostic tool for the treatment of depression.
“We can now predict who is likely to recover on antidepressants in a way that takes into account their life history.”
The researchers envision the integrated clinic of the future in which physicians ask about childhood trauma and order a five-minute brain scan to help determine the best line of treatment.
The study also provides a table that the researchers say could ultimately be used by practicing physicians to determine the threshold at which antidepressant treatment is recommended depending on patients’ varying levels of ELS and brain-scan results.
Better depression diagnostics could make a significant impact of the community burden that results from the disease, and decrease the suffering of those affected.
Reference:
- Andrea N. Goldstein-Piekarski, et al. Human amygdala engagement moderated by early life stress exposure is a biobehavioral target for predicting recovery on antidepressants. PNAS; doi: 10.1073/pnas.1606671113
Last Updated on February 17, 2023