Olfactory ensheathing cells, also referred to as olfactory ensheathing glia, are a type of radial glia found in the nervous system. They are also known as olfactory Schwann cells because they ensheath the non-myelinated axons of olfactory neurons in a similar way to which Schwann cells ensheath non-myelinated peripheral neurons. They also share the property of assisting axonal regeneration.
The transplantation of olfactory ensheathing cells (OECs) into the damaged area is one approach to restoring function after spinal cord injury currently being explored. The hope is that the transplanted cells will encourage the repair of damaged neurons.
But does it work? And if so, how can it be optimized?
Spinal cord injuries are mostly caused by trauma, often incurred in road traffic or sporting incidents, often with devastating and irreversible consequences, and unfortunately having a relatively high prevalence. The figures are as high as 250,000 current patients in the USA; 80% of which are male.
According to a systematic analysis of the literature published recently in PLOS Biology, after experimental spinal cord injury, transplanting olfactory ensheathing cells into the site of damage does indeed significantly improve locomotor performance.
To reach this conclusion, Ralf Watzlawick, Jan Schwab, and their colleagues at the Ohio State University Wexner Medical Center, Charité Universtaetsmedizin Berlin and the CAMARADES consortium (Collaborative Approach to Meta Analysis and Review of Animal Data from Experimental Studies), analyzed 49 studies, published between 1949 and 2014, which included 62 experiments involving 1164 animals.
Formidable Challenge
Restoration of function after spinal cord injury remains one of the most formidable challenges in regenerative medicine, but cell transplantation into the spinal cord represents a promising treatment strategy.
OECs are considered particularly suitable for transplantation because they have been shown to be neuro-protective and to promote neuro-regeneration in different settings, and can be extracted from the patient’s own nasal cavity, thereby minimizing the chances of graft rejection and avoiding the need for immunosuppressive drugs.
The mammalian olfactory system is unusual in that it has the ability to regenerate its neurons during adulthood continuously. This ability is associated with olfactory ensheathing glia. New olfactory receptor neurons must project their axons through the central nervous system to an olfactory bulb in order to be functional.
The growth and regeneration of olfactory axons can be attributable to OEG, as they form the fascicles through which axons grow from the peripheral nervous system into the central nervous system. Olfactory receptor neurons have an average lifespan of 6–8 weeks and therefore must be replaced by cells differentiated from the stem cells that are within a layer at the nearby epithelium’s base.
Axonal growth is guided by the glial composition and cytoarchitecture of the olfactory bulb in addition to the presence of olfactory ensheathing cells.
Results Contradictory
Reports in the literature about the efficacy of transplantation of OECs for treatment of spinal cord injury have been contradictory.
Therefore, to investigate the in vivo evidence for the efficacy of this procedure, the authors implemented a systematic review and meta-analysis of the literature. Importantly, the authors set out to explore the potential influence of variations in experimental approaches and unreported data.
“We felt that after more than two decades since the discovery that OECs elicit effects on neural plasticity in vivo, it was time to test their effects by appropriate methodology beyond reproduction,” the authors argued.
The data analysed by the authors justify the use of OECs as a cellular substrate to develop and to optimize minimally invasive and secure protocols for repairing damaged spinal cord.
They also identified several aspects of the cell transplantation procedure that could have a significant impact on the size of the therapeutic effect, including:
- the time-point of the application
- the use of surgical micro-dissection to “refresh” the scar tissue
- the localization of transplanted cells
- the number of injections
- the injected volume
- the dose of cells administered
Importantly, by using state-of-the-art statistical methods the authors also found that the impact of publication bias (due to selective failure to report results) was minimal, further supporting the translational potential of this approach.
Despite being focused on OECs, the findings may be of more general relevance for optimizing the transplantation of other cell types after spinal cord injury.
Reference:
- Ralf Watzlawick, Julian Rind, Emily S. Sena, Benedikt Brommer, Tian Zhang, Marcel A. Kopp, Ulrich Dirnagl, Malcolm R. Macleod, David W. Howells, Jan M. Schwab. Olfactory Ensheathing Cell Transplantation in Experimental Spinal Cord Injury: Effect size and Reporting Bias of 62 Experimental Treatments: A Systematic Review and Meta-Analysis. PLOS Biology, 2016; 14 (5): e1002468 DOI: 10.1371/journal.pbio.1002468
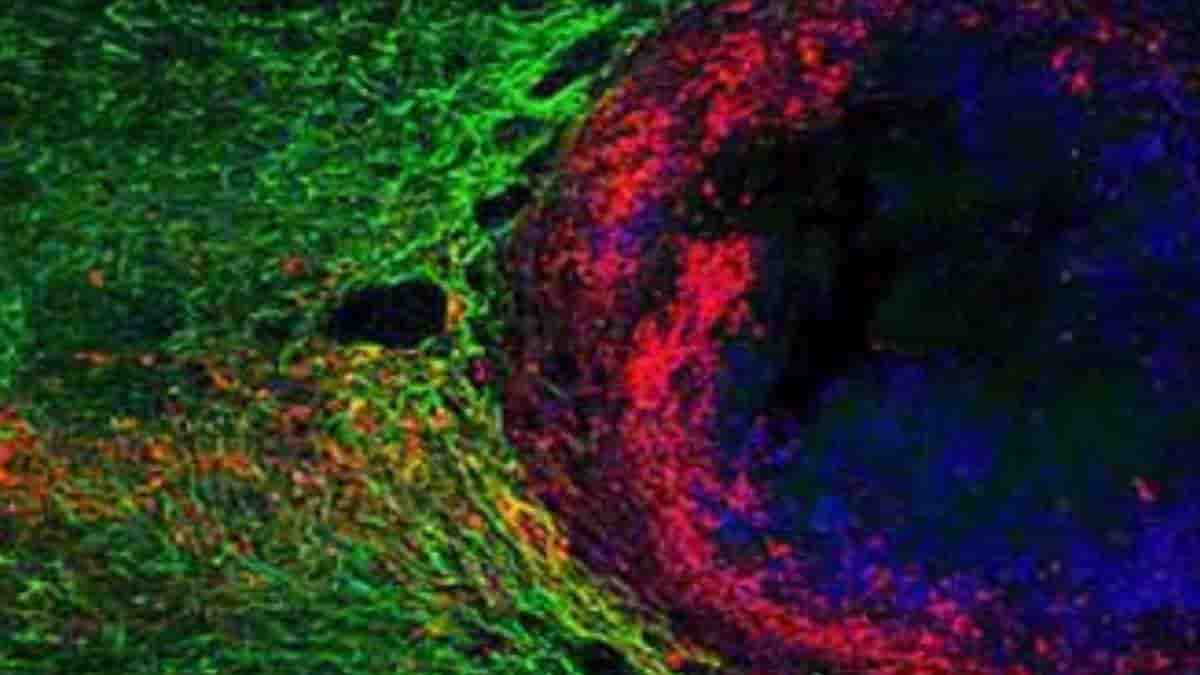
Image: Previously injured axons (in red) can grow through a dense astrocyte scar (in green) in the presence of molecules that stimulate growth (in blue). Credit: Dr. Michael V. Sofroniew, UCLA.
Last Updated on October 20, 2023